Preparing for Surgery
The run up to surgery can be a real roller coaster experience - not knowing what to expect, how to feel and even questioning ‘Am I doing the right thing?’. You are not alone - many have gone before you and have had the same worries, concerns and feelings. In this section we will talk you through how to prepare emotionally and practically for surgery.
What to expect at a ‘pre-op’ appointment
What can I do for myself to prepare for surgical recovery?
What are the different types of surgery and do they leave scars?
What do I need to pack for the hospital?
Where can I find support during this time?
Can I change my mind about having the surgery?
How soon after surgery can/should I start HRT?
For more in-depth information and answers to commonly asked questions you can also visit our searchable knowledge base here:
What to expect at a pre-op appointment
Going to the pre-op appointment can be daunting and many people worry as they do not know what to expect if they have not had surgery before.
The pre-op appointment helps everyone to prepare you safely for your procedure or operation, and identify any areas where can help improve with your general health before having an anaesthetic. In order for the hospital to safely assess your suitability for the surgery, they will need to learn about your medical and surgical history, any medication (and supplements) that you are taking, and any previous medical issues.
On the day of your appointment it may be helpful to bring with you:
A written list or prescription of your medications (and supplements)
A list of your previous operations or illnesses (do not worry if you cannot recall the exact dates)
Any previous copies of hospital doctors’ letters if you have them available
Your contact details and details of your doctor(s)
A written list of any questions/concerns you have - it can also help to take some paper and a pen to jot down answers at the time, as it is easy to forget the details.
On your arrival at the clinic, you will be asked to confirm your name, address, contact details and GP details.
In your appointment a healthcare assistant will do routine observations such as your height, weight, blood pressure, heart rate (ECG) and you may have some routine skin swabs taken. Some patients may also require a urine sample.
You will usually have a consultation where a health care provider will take a detailed medical history from you. The whole assessment usually lasts under an hour. However, if you have a complicated medical history and/or need additional tests, it may run a little longer.
Each hospital will have their own way of doing things - if you are particularly nervous, ring ahead and ask them to explain what is covered at a pre-op. Many hospitals also have details on their website so you can it look up ahead of time to calm your nerves.
If I am on hormone replacement therapy (HRT) or ovarian suppression treatments (i.e., GnRH analogue) do I need to stop it to have the surgery?
Many individuals with PMDD/PME who are about to undergo surgical menopause are already taking medications that influence their hormone levels prior to surgery. This can include GnRH analogues (which create a temporary chemical menopause), estrogen, and/or progesterone. For those with certain gynecologic conditions (e.g., uterine fibroids), GnRH agonists are frequently used prior to hysterectomy/oophorectomy to reduce uterine enlargement and related symptoms (e.g., due to fibroids). Therefore, most surgeons are accustomed to patients being on GnRH agonists leading up to surgery.
GnRH analogues can be continued on schedule prior to surgery in order to minimize the impact of surgery on hormone flux. This may be especially indicated for those who are using GnRH analogues to treat a brain hormone sensitivity (e.g., PMDD, PME). As always, it is important to discuss this issue with your medical professionals to determine what is right for you.
Estrogen HRT
Many individuals who are being treated with GnRH analogues also take estrogen and progesterone hormone addback to prevent menopausal symptoms and risks. Because estrogens can increase the risk of blood clots, some surgeons may recommend discontinuing HRT prior to surgery. This may be dependent on how you are taking estrogen. Transdermal estradiol patches have been found to show lower risk of blood clots than other types of estrogen HRT, and this option may be more acceptable to your surgeon. Be sure to discuss this topic with your medical professionals to determine what is right for you.
What can I do for myself to prepare for surgical recovery?
Oophorectomy (plus hysterectomy) is a major surgery, and recovery can be a complex process. Being psychologically and physically prepared is key. You can help make it easier for yourself by preparing your home and organizing extra help in advance.
Fellow patients who have been through the surgery kindy offered their advice for preparing in advance. Including ‘Handy items for recovery’ and ‘preparing your home’ for an easier recovery.
You not need to shave or wax your public hair especially for surgery. In fact, it is recommended that you avoid shaving pubic hair pre-surgery since any nicks in the skin from the razor can make you more vulnerable to infection. Gynecological surgeons see vulvas of all shapes, sizes and hairiness every day so you do not need worry! Also - you can still have the surgery if you are on your period so don’t worry if your op date falls when you are bleeding - they have seen it all before!
What are the different types of surgery and do they leave scars?
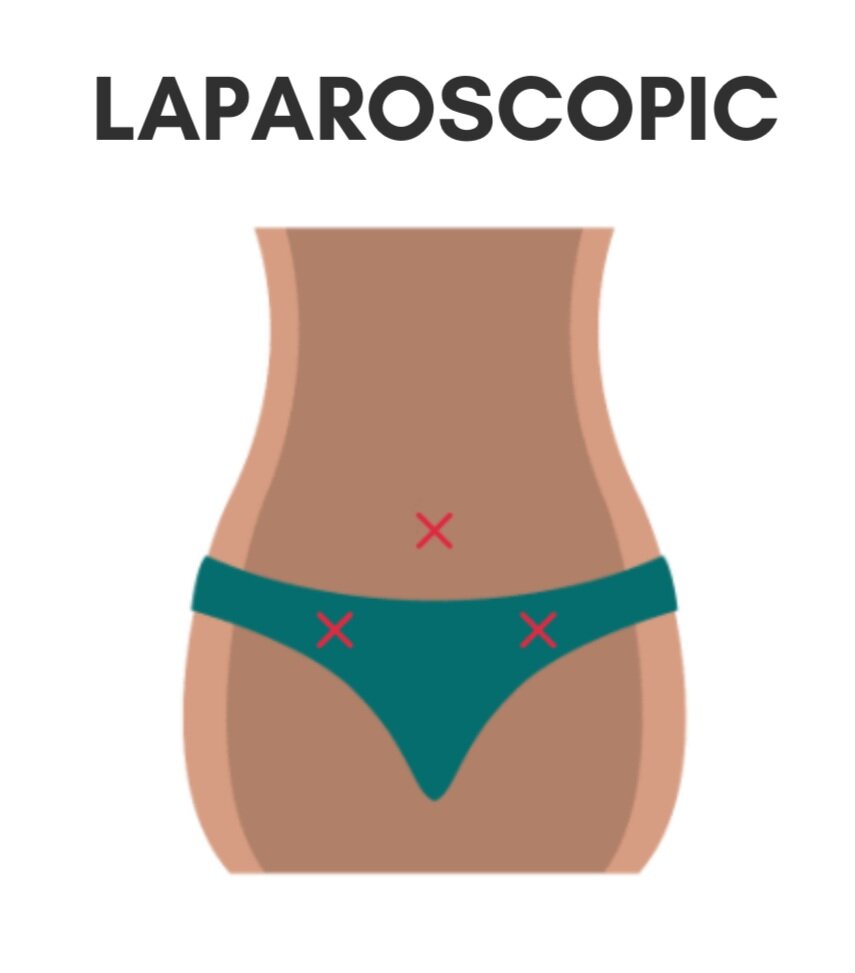
Laparoscopic Surgery
How it works: During the procedure, a small tube containing a telescope (laparoscope) and a tiny video camera will be inserted through a small cut (incision) in your abdomen. This allows the surgeon to see your internal organs. Instruments are then inserted through other small incisions in your abdomen or vagina to remove your uterus, cervix and any other parts of your reproductive system. These laparoscopic surgeries are usually carried out using general anaesthetic– where you'll be unconscious during the procedure..
Who is it usually recommended for?: Laparoscopic surgery is also known as keyhole surgery. It's the preferred way for most patients to remove the organs and surrounding tissues of the reproductive system.
Healing and Recovery: This method is the most common since it is the least invasive, and therefore has a shorter hospital stay and faster recovery time. There is also generally less pain and bleeding after the operation, and reduced scarring relative to abdominal surgery.
Vaginal Surgery
How it works: During a vaginal hysterectomy, the uterus and cervix are removed through an incision that's made at the top of the vagina. Special surgical instruments are inserted into the vagina to detach the uterus from the ligaments that hold it in place. After the uterus and cervix have been removed, the incision will be sewn up. The operation usually takes about an hour to complete. A vaginal hysterectomy can either be carried out using general anesthetic – where you'll be unconscious during the procedure.
Who is it usually recommended for?: A vaginal hysterectomy is usually preferred over an abdominal surgery as it's less invasive.
Healing and Recovery: Because this method is less invasive than abdominal surgery, it generally involves a shorter stay in the hospital, and the recovery time tends to be quicker than abdominal surgery. There is less scarring relative to abdominal surgery.
Laparoscopic Assisted Vaginal Surgery
This approach combines both techniques of a laparoscopic and vaginal approach. This may be the preferred approach for some gynecologists and has the same benefits of a purely laparoscopic approach.
Abdominal Surgery
How it works: During abdominal surgery, an incision will be made in your abdomen. It will either be made horizontally along your bikini line or vertically from your belly button to your bikini line. A vertical incision will usually be used if there are large fibroids (non-cancerous growths) in your uterus, or for some types of cancer. After your uterus and/or ovaries have been removed, the incision is stitched up. The operation takes about two hours to perform and a general anesthetic is used.
Who is it usually recommended for? An abdominal hysterectomy may be recommended if your uterus is enlarged by fibroids or pelvic tumors and it's not possible to remove it through your vagina.
Healing and Recovery: Abdominal surgery is the most invasive method, and may result in more delayed recovery times and scarring.
Further reading about different approaches and their relative risks and benefits: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC558455/
What do I need to pack for the hospital?
The length of you stay in hospital will depend on your health care system and also if your surgery goes smoothly. Some people may need more recovery time than others. However, most people tend to agree that they packed far too much - so it’s best to pack light and focused! With this in mind, our IAPMD surgical menopause patient insight team helped collate this free, downloadable packing list to keep you comfortable and prepared.
Where can I find support during this time?
Support when going through this time is really important - it can be real upheaval both physically, emotionally and mentally so do not suffer alone.
Additional support pre and post-surgery
Depending on your reason for having the surgery, some people find that they need additional emotional support in coming to terms with being ‘post-op’ (post-surgical operation). In particular, loss of fertility can be very difficult for those who had wanted to maintain the option of “natural” pregnancy. Others may find they are traumatized by what led them to have surgery (e.g., in the case of PMDD, this may be years of severe emotional or behavioral symptoms).
Some people find that talk therapy (either supportive counseling or cognitive-behavioral psychotherapy) is useful for addressing grief or emotional symptoms that may arise during your transition into surgical menopause. If you’re unsure where to start, search for a “cognitive behavior therapy” in your area. Your doctor may also have recommendations.
Peer support
Peer support can be very useful - speaking to those who have been through, or are going through similar situations can be a relief for many. Below, we list several of the available online resources:
PMDD, Hysterectomy, oophorectomy and life after - IAPMD
IAPMD peer support - free one-to-one support for those with hormonal sensitivities such as PMDD /PME.
INSPIRE - a non-social media community where you can interact with others (anonymously if prefered). Download the app here (currently not available on Android).
The above services are run by IAPMD. The following resources may be useful but are not affiliated with IAPMD:
For additional support and information around primary ovarian insufficiency (POI) you can visit The Daisy Network.
Menopause cafes are becoming popular in the UK and around the world - A Menopause Cafe is a group directed discussion of menopause with no agenda, objectives or themes. It is a discussion group rather than a support or counselling session. You can even start your own local group if there are none near you yet!
Surgical Menopause Support group (Surmeno Connection) - Facebook (not PMDD specific)
Surgical Menopause UK Support group - Facebook (not PMDD specific)
How soon after surgery can/should I start HRT?
While there are no studies directly comparing the timing of HRT initiation following surgical menopause, the dosage and timing of HRT should be discussed with your surgeon prior to the operation. Some doctors we surveyed reported that they prefer to begin HRT as soon as the patient leaves the hospital (provided medical safety for the individual patient). Studies suggest that HRT is underused in surgical menopause, and so it is important to have discussions with your doctor prior to surgery about how you will work together to optimize HRT in surgical menopause.
Can I change my mind about having the surgery?
Yes! It is your body and ultimately your decision. You are entitled to change your mind even at the last minute. If you are having concerns, it is best to talk your reasons and worries through with a trusted friend, and also your doctor. It is extremely normal to be worried about the surgery and the outcomes - but if you feel your worries are more than ‘last minute jitters’ then do ensure you speak to people who can help you. Do not let anyone push you into having major surgery if you feel it is not right (or not the right time) for you and your circumstances.
For more in-depth information and answers to commonly asked questions you can also visit our searchable knowledge base here:
This project was financially assisted by The Patty Brisben Foundation for Women’s Sexual Health. The views expressed herein do not necessarily represent those of The Patty Brisben Foundation for Women's Sexual Health.